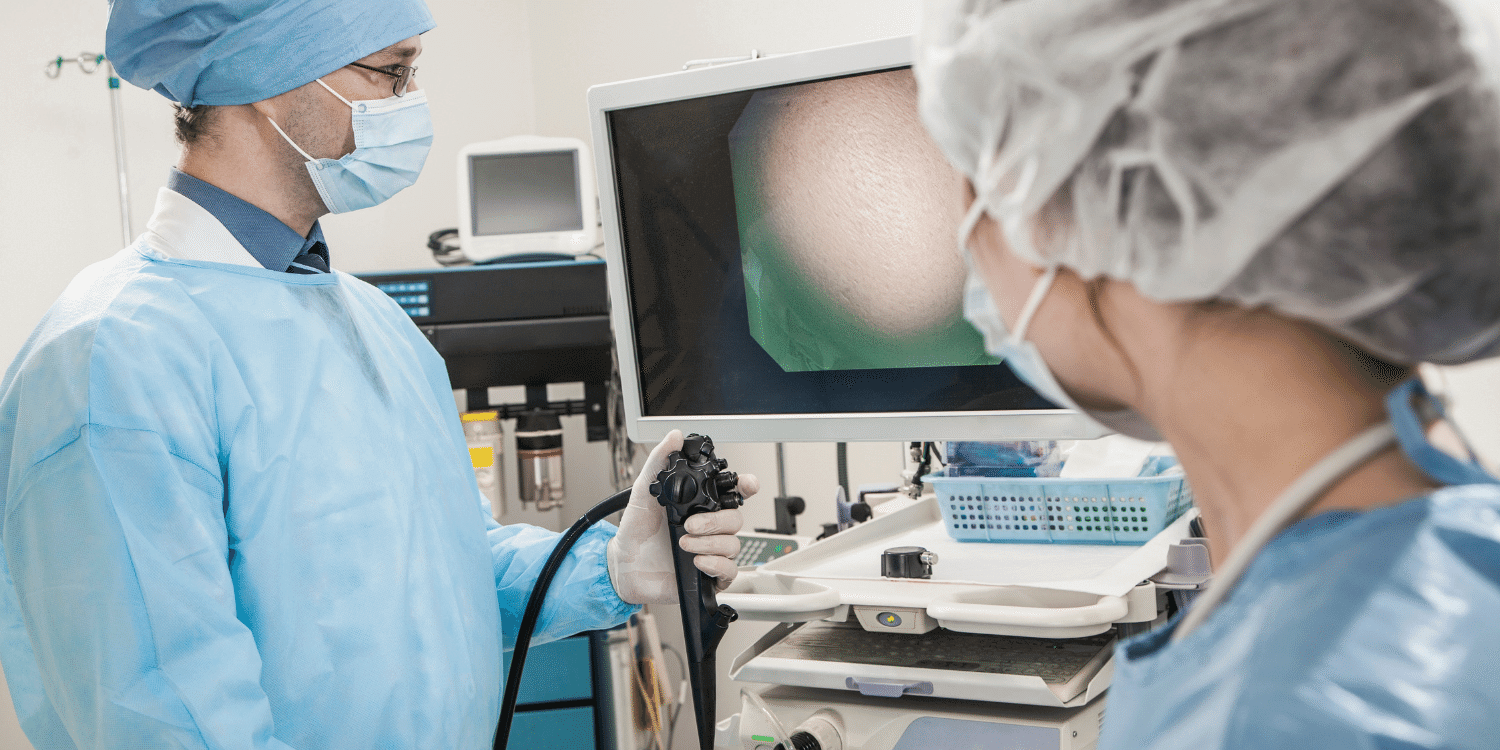
Reasons why there is no need to be scared of endoscopy
What are the most common examinations performed when diagnosing disorders in digestive organs?
Before planning any examinations and tests, it is important to talk to the patient, find out about current symptoms and his medical case history. Based on that, a patient will receive an individualised plan of laboratory and instrumental tests. The main instrumental examinations applied for diagnostics of intestinal disorders include pelvic ultrasound, upper gastrointestinal endoscopy, and endoscopic examination of the large bowel (also known as colonoscopy).
What is an endoscopic examination of the large bowel and colonoscopy?
The upper gastrointestinal examination is a procedure performed using a special endoscope to examine the oesophagus, stomach, and the upper small bowel called duodenum. Meanwhile, a colonoscopy is a procedure that enables an examiner to evaluate the inside of the colon (large bowel) with an endoscope (a special flexible tube).
Why is a colonoscopy performed?
The upper gastrointestinal endoscopic examination must be done if you have pain or any type of discomfort in the upper part of the stomach. In case previous treatments bring no results. Or in case of any “dangerous” symptoms, such as, newly occurred symptoms in people of 50-55 years or older; if any of your relatives had stomach or oesophagus cancer; weight loss, bleeding, difficulties with swallowing or painful swallowing, iron-deficiency anemia of unknown origin, chronic vomiting, palpated mass in the stomach or enlarged lymph nodes, jaundice. This type of examination is also recommended when a patient experiences difficulty in swallowing or endures painful swallowing, has recurring or long-term gastroesophageal reflux disease, vomiting of unknown origin, an iron deficit, or abnormal tissues diagnosed by other radiological examinations. The examination can also be performed as part of a treatment.
A colonoscopy can be performed as part of a routine screening (Programme for Early Detection of Large Bowel Cancer), as a follow-up examination for patients with inflammatory bowel diseases, after resected polyps and large bowel cancer, or for the assessment of expansion of inflammatory bowel diseases. This examination can also be useful in patients with active or chronic bleeding (unknown reason of iron-deficit anaemia), chronic complaints of pelvic pain for unknown reasons (for example, chronic diarrhoea), sudden changes in the nature of defecation (constipation along with other dangerous signals like weight loss, anaemia, blood in faeces) or abnormal tissues diagnosed by other radiological examinations.
The upper gastrointestinal endoscopic examination and a colonoscopy can be performed as part of a treatment.
What is the course of these examinations and how to prepare for them?
Before performing any examinations, each patient receives information on the course of the procedure, about the possible discomfort she can feel and the actions that can be taken to reduce discomfort. The patient’s confidence in his doctor and the examination technique to be performed by a qualified specialist are very important for the success of the procedure. This is a very specific examination, which requires an experienced doctor. The more accurately the examination is performed, the better the evaluation of pathological tissues. When a patient is being prepared for these examinations, he receives all the information about possible complications and signs a consent form. If a patient refuses the examination, it is not performed.
You must not eat at least 6 hours before your procedure. For people with prolonged bowel evacuation it is recommended to avoid eating for even longer periods. In the morning, you can take your medications (to reduce blood pressure, for example) with a little water. If a patient has diabetes, an examination should be performed in the morning. Otherwise, you will need to adjust the time of the drugs prescription. If a patient takes medicines affecting the blood´s clotting ability (aspirin or clopidogrel), it is necessary to evaluate the risks of thrombosis. It is recommended to avoid taking these drugs for at least 5 days before a colonoscopy.
The preparation of your bowel for a colonoscopy plays an important role. Usually, the preparation begins a day before the procedure. You will need to drink special liquids to clean your colon. If a colonoscopy is scheduled in the afternoon, it is recommended to drink half of the liquid in the evening, while the other half early in the morning (the day of the exam).
Many patients dread endoscopic examinations because of discomfort. Are there any ways to avoid it?
Although endoscopic examinations may seem unpleasant, they are necessary to diagnose the disease in early stages and apply successful treatment. Also, the discomfort experienced during the procedure can nowadays be suppressed with the help of medicines.
Regecting a foreign body is a natural human reflex. The degree of sensitiveness varies among people, as does the pain threshold. Anyway, a patient receives a local spray anaesthetic (lidocaine) into the throat before the upper GI endoscopic exam. Some patients unreasonably dread these exams, but endure them quite easily. While other patients aren’t afraid of the exam at all, follow the instructions, but their vomiting reflex is so strong that it makes the procedure more difficult to perform. Such patients receive a short-term intravenous anaesthesia. This general anaesthesia lasts only a few minutes. Doctors use special medicines that have a short-term effect with no adverse reactions.
The pain threshold to a colonoscopy depends on the patient bowel’s anatomy. The bowels may be bent or twisted thus it could be difficult to access them. The movement of the endoscope through the bowels become complicated due to clots formed after pelvic surgeries. At Northway Medical and Surgical Centre, this examination in all cases is performed under a general intervenous anaesthesia, so the patient feels nothing.
What kind of abnormalities can be detected during these examinations?
The upper gastrointestinal endoscopic exam can help diagnose both malignant and non-malignant diseases or make sure no pathology is present. Non-malignant diseases include oesophageal erosions, stomach erosions, duodenal erosions, ulcers, and inflammatory changes of various origins in the stomach´s mucose membrane. It also helps to diagnose malignant, i.e. cancerous diseases.
Usually, a colonoscopy helps to diagnose polyps. More rarely, diverticulum, large bowel cancer, and inflammatory bowel diseases. Apart from the visual examination, the doctor may take a sample to be sent to a pathologist for a biopsy.
What kind of endoscopic treatment can be applied?
These examinations can be applied during various treatments. It mostly depends on the healthcare specialist’s qualification and equipment capabilities. The most common endoscopic treatment methods include resection of polyps in the large bowel, resection of stomach polyps, pre-cancerous tissues and early stomach cancer, expansion of narrowed lumina, stent placement, bleeding control, and removal of foreign bodies from the oesophagus.
Are these examinations safe? Yes, these examinations are safe, especially when carried out as part of prevention. The risk of complications is very low. The frequency of the appearance of complications during the endoscopy of the upper GI is 0.1%, while during a colonoscopy it is 0.3%. The frequency of complications when using endoscopies for treatment is higher and depends on the nature of the treatment method.